Scope, Conceptualization & Strengthening of Mental Health Services at Ayushman Bharat Health and Wellness Centers
Mental health is by far neglected in developing countries, as the focus of public health care delivery has primarily been physical health. We, therefore, find ourselves challenged at the hands of Mental health disorders.
Introduction
India has witnessed exponential growth in the field of medical science in the past decade. Starting from the grassroots level, we have reached the masses, and have successfully treated various diseases that cause early morbidities and mortalities. In developing countries, the focus of public health care delivery has primarily been physical health. Despite being at the epitome of medical sophistication we find ourselves challenged at the hands of Mental health disorders. WHO defines Mental health as a state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, and work productively as well as fruitfully, and can contribute to his or her community. Therefore, these disorders are often crippling and affect an individual's personal, social, and economic life. WHO has added protection of mental health under Sustainable Development Goal (SDG-3) as a target to be achieved by the year 2030. Mental, Neurological, and Substance use (MNS) disorders lack a definite course of treatment and need a rather holistic approach, making it challenging and prolonging their treatment time. The national mental health survey (2015-2016) conducted by NIMHANS was able to capture the increasing burden of MNS disorders. The survey gives a comprehensive understanding of the prevalence of various types of MNS Disorders. According to the reports, the lifetime prevalence for any mental morbidity was 13.7% and one-year prevalence was 10.6%, which is equivalent to approximately 15 crore people. The survey also reported the treatment gap ranges between 70% and 92% for different mental disorders. The number is significantly large and worrisome and indicates an array of barriers evoking low utility of services among the affected population.
Existing Mental Healthcare System
In its efforts to address the lack of a mental healthcare system, India has witnessed various remarkable movements. Until the mid-1900s Mental health services existed only in big cities, but that scenario is slowly changing.
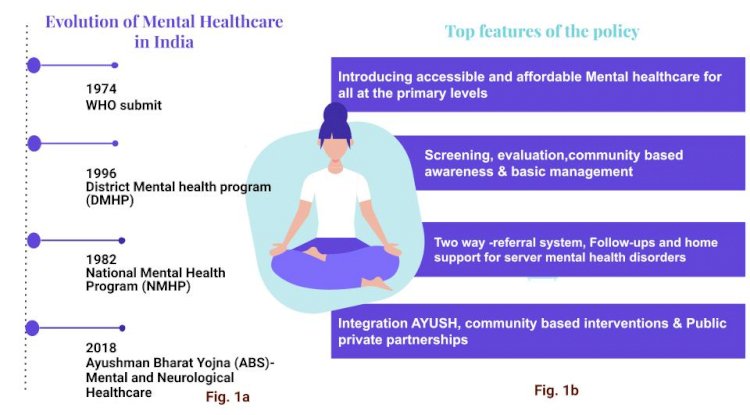
Over the years commendable recommendations have been made to improve mental healthcare, but the implementation seems to be lacking. India was one of the first countries to adopt the National Mental Health Program (NMHP). The WHO’s meeting on “organization of mental health services in developing countries” in 1974 at Addis Ababa was a landmark event in the history of mental healthcare in developing countries. It led to the launch of ‘Strategies for Extending Mental Health Care’ (1975–1981) and the plan was to implement mental healthcare along with general healthcare in the seven developing countries. This proposal was also in line with the Alma Ata declaration ‘Health for all, ‘All for health’. Institutes like the National Institute of Mental Health and Neurosciences (NIMHANS) and Post Graduate Institute of Medical Education and Research (PGIMER) were pioneering the research and providing technical guidance to decentralize mental health care.
This was a paradigm shift movement in history to achieve universal coverage for mental health care. Even though the research carried out by PGIMER and ICMR-DST suggested that 20% of cases could be identified and successfully reported by training PHC staff on Mental and Neurological health care, it was realized that operationalization of mental health at the PHC level would be difficult therefore the program was moved to the district level, forming the District Mental Health Program (DMHP). The NMHP and DMHP were the first of their kind covering an array of health conditions under a single program. The objective of NMHP was to integrate mental health care along with general health care, empower and increase community participation, and lastly to ensure the availability and accessibility of some form of mental healthcare, particularly to the most vulnerable and underprivileged population. Despite being a revolutionary step towards achieving mental health care for all, a 2008 evaluation pointed out many bottlenecks that resulted in the failure of this policy. These failures were a result of pre-existing weakness within the primary healthcare system besides factors such as lack of meticulous monitoring, evaluation and training system, shortage of drugs, human resources, and treatment delays due to societal factors. (Mahajan et. al. 2019). There is a shortage of doctors in PHC (8%), specialists at CHC (65%), and other health workers both M/F. (Kumar, 2011). Apart from this the DMHP is only operational in 125 districts out of 626 districts and almost dysfunctional at the primary level which leaves a majority of the population uncatered for. To address these inefficiencies the Government of India’s Ministry of Health and Family Welfare (MOHFW) launched Ayushman Bharat Yojana (ABS)- National health protection Mission in September 2018.
FLOW OF SERVICES
Ayushman Bharat Scheme (ABS)
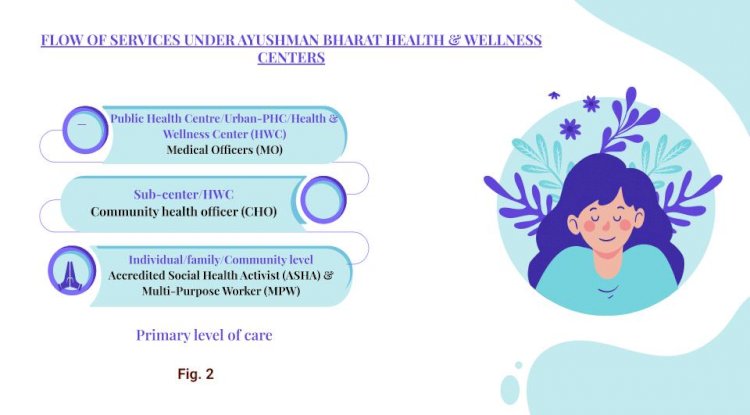
Rural areas are undeniably more vulnerable to MNS disorders due to poor literacy levels and health infrastructure, they face a catastrophic burden of Mental illnesses. The objective of ABS is to provide comprehensive and quality care at the PHC level as well as to integrate preventive, promotive, curative, rehabilitative, and palliative care at doorsteps. To meet this goal the Government plans to revamp most sub-centers and selected PHCs to Health and Wellness Centers (HWC). These HWCs will provide an expanded scope of services. A list of comprehensive guidelines covering all scopes of healthcare including mental health were rolled out by the MOHFW. The AB-HWC (Ayushman Bharat Health and Wellness Centres) paradigm plans to further decentralize the mental healthcare system making provision of care at community and sub-center/PHC level. In the following paper, we will analyze the conceptualization and strengthening of mental healthcare services at Ayushman Bharat Health and Wellness Centers.
Mental Health care at Ayushman Bharat Health and Wellness Centers
Operational Guidelines- Mental, Neurological, and Substance Use (MNS) Disorders Care at Health and Wellness Centers functions and is supplementary to the National and District Mental Health Programs. The recommendation of this policy is based on the learning of DMHP. The strategy to achieve mental health is through a continuum of care starting from the primary level to the secondary and tertiary level of care and through promotive and preventive activities. (Figure-1)
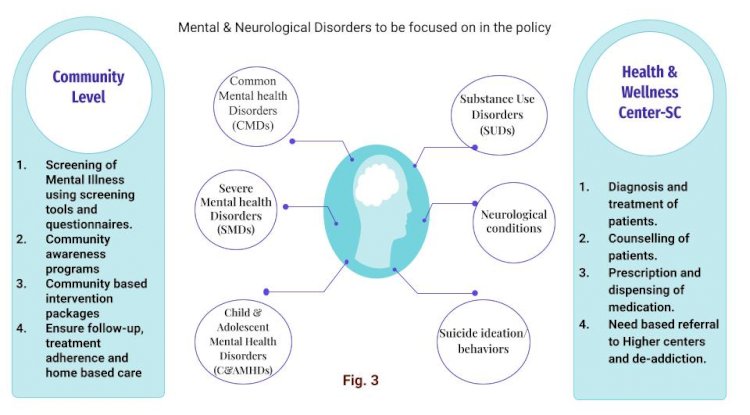
The focus of the policy is on six groups of MNS disorders:
- Common Mental Health Disorders (CMDs)
- Substance Use Disorders (SUDs)
- Neurological conditions
- Severe Mental Health Disorders (SMDs)
- Child & Adolescent Mental Health Disorders (C&AMHDs)
- Suicide Ideation/Behavior
Expectations of care as per the guidelines
Primary care largely involves improving community awareness on mental health disorders and to reduce the stigma around them. Mental health conditions should be viewed as another disorder that can very well be treated. The Primary level healthcare team will comprise of ASHAs, Multi-Purpose Workers F/M (MPWs), Community Health Officer (CHO), Staff Nurses, and a Medical Officer (MO). They will be involved in all activities from identification to delivery of mental health care services.
At grassroots or individual/family/community level
ASHAs and MPWs will be responsible for mobilizing the community disseminating knowledge, raising awareness, tackling stigma as well as identifying patients for Depression, Psychosis, Epilepsy, Alcohol use disorder, and Behavioral problems using Community Informant Decision Tool (CIDT). ASHAs and MPWs will be responsible for the early identification and reporting of MNS disorders. They will also be trained to provide community-based intervention packages (e.g., relaxation training, psychological first aid, basic guidance on self-care) to those who screen positive. Information, education, and Communication (IEC) tools will be used to promote health for behavior change communication. For further intervention, patients will be referred to CHO at Sub-center/HWC.
At the sub-center/HWC
An addition of a CHO has been done on this level. S/he will be responsible for providing primary level care to individuals at this level. S/He will undertake awareness, screening, and management activities. S/He will provide psychosocial intervention for CMDs, SMDs, SUDs, and C&AMHDs and refer them further according to the patient's needs. For patients with epilepsy and dementia, CHO will screen and refer them to PHCs/UPHC, where they will be diagnosed and provided pharmacological management by MO. A comprehensive life plan and management of the general well-being of the family as well as of the patients suffering from dementia is suggested. Individuals will also be assessed for depression using a Patient Health Questionnaire (PHQ) 9 and assessed on risks of suicide. CHO will not be authorized to prescribe medication but shall dispense the already prescribed medications from MO or psychiatrists. S/He will also look for signs of toxicity of prescribed medication. In short, a CHO will be the eyes, ears, and hands of the community. S/He will ensure the availability of mental health care to patients at his level and refer those in need to higher levels and make sure the patients adhere to the treatment.
At the PHC/UPHC/HWC
Apart from the other dimensions of care, MO will provide pharmacological and psychosocial care to patients referred from sub-center/PHC/HWC as well as those who directly enter at this level for all mental illnesses. Diagnostic tools for Epilepsy and Dementia Assessment by Rapid Test (DART) will be used by MO to screen patients. While the general treatment for CMD, SMD, SUDs in adolescence will remain the same, treatment will be tailored to best suit individuals. The MO for further care will refer the patients to a pediatrician/physician, psychiatrist, or clinical psychologist at DMHP/STC. Emergency care for seizures and assessment of other conditions will also be done at this level. Those cured will be discharged and others will receive follow-up care and shall be referred back to sub-level where ASHA/MPW will provide follow-up at home and ensure adherence to treatment and support. The main objective of this back and forth is to provide a continuum of care and eradicate treatment gaps.
Preventive and promotive
Mass awareness programs focused on group discussions and one-on-one interactions will be done to reinforce preventive and promotive activities. Patients will be encouraged to talk about their feelings in a safe environment, receive comfort and reassurance from the HCW. They will be encouraged to perform self-care routines. The counseling methodology used will involve empathic listening and reflection as well as behavioral activation and problem-solving techniques. They will also be counseled to manage relapse, peer pressure, and handle emotions. Mobile Medical units will also be made available to ensure service delivery to the remotest areas adding to the provision of providing a Continuum of care.
Training of Health Care Workers (HCWs)
The policy recognizes the need for skillful training and has provision for it. All primary healthcare workforce will be trained by a DMPH psychologist. The model used here will be a training of trainer’s (TOT) model. Medical officers will play the role of master trainers and further train MPW, Staff nurses & CHO. ASHAs will be trained on identification, health promotion, and the stigma associated with MNS. She will also be given training on providing extended care packages. Program managers will also be given a single day of training to bring them on speed on the dispersion of care such as ensuring availability of drugs as well as monitoring and supervision.
Alliances
CHO is also provisioned to arrange for community and school health programs (E.g., Yoga & other physical activities), and partnership with NGOs, faith healers, and government departments for promotive and referral of MNS related services. It integrates programs like Rashtriya Bal Swasthya Karyakram (RBSK) and Rashtriya Kishor Swasthya Karyakram (RKSK) to ensure the well-being of children. The policy also plans to integrate AYUSH doctors at the primary health level. He will provide Ayurvedic medicines and remedies for patients who wish to discontinue allopathic medicines. He will also be able to discharge common drugs based on the Essential Drug List (EDL).
Monitoring
Data shall be collected regarding all aspects of MNS at each level. The National Health Management Information System (HMIS) will now integrate data monitoring systems for MNS disorders.
A Policy Analysis
The policy brings few distinctive features to the table and seems to address the shortcomings of DMHP. To begin with, ABS is the largest formal effort ensuring the mental well-being of all starting from the grass-roots level by integrating mental health care along with general health care at the HWCs. The second feature of this policy is the training of ASHA, MPW, CHO, and MO by a DMHP psychologist to identify and treat persons with mental illnesses. This concept is also known as ‘task shifting’, where roles are shifted from the higher specialized workforce to the lower specialized workforce to improve the efficiency of the system.
The policy also talks about integrating AYUSH medicine and tools of yoga and naturopathy which has proved to be effective in helping persons with CMD. The two-way referral system is another feature of this policy where patients will be referred up to higher centers based on their needs and back referred to lower centers to ensure treatment adherence and monitoring. Active communication between healthcare providers at the different tiers will close the loop enforcing a continuum of care which will create a responsive system with better management of patients with mental illnesses in health centers as well as the community. Lack of medication was also recognized as one of the bottlenecks of DMHP. The ABS would maintain medicine supply as per the essential drug list (EDL) at all levels.
The policy also includes the use of Information Education Communication (ICE) material to encourage positive mental health and behavior change at the community level. The primary health care team, headed by the CHO will be in charge. Mental health programs will be integrated along with village and school intervention programs to spread awareness along with campaigns, group sessions, and peer-support groups will also be held for community mobilization.
It was hoped that AB-HWCs would be an ambitious and innovative effort towards achieving mental health care for all. This policy seems to cover everything that was lacking in the previous policies. The AB-HWC paradigm aims to decentralize mental health care, in theory, it might appear practical, yet the foresight required to implement such a program is missing. Due to the complexities and diverse nature of the country, a single system to flourish is impossible. Prior efforts to implement such a program (NMHP) at the primary level have failed, which suggests the success of ABS will mainly depend on the collective effort of its stakeholders, the motivation of states, and the healthcare workforce.
Let us dive deeper into the role of HCWs. At the primary level, care will largely be subjected to the skill and motivation of the healthcare workers. Thought needs to be given to the role of ASHAs. ASHA workers are the members of the community and therefore act as health advocates. ASHA’s are an excellent intervention but the recent narrative has brought to light the dissatisfaction and overburdened plight of them. They are scarcely paid and reap the low benefits of their work. With this in mind, we need to evaluate if it is reasonable to burden them with additional responsibility and how will this affect the performance of already demotivated ASHAs and the outcome of this policy?
The addition of Community Health Officers (CHOs) and ASHAs can also prove to be very beneficial in identifying and treating persons with common mental illnesses. But managing severe mental illness will be a difficult task as they lack the experience needed to treat them. CHOs like ASHA will take care of the general health as well as the mental health of patients. Individuals tend to form bonds with these officers and feel comfortable sharing their issues or bringing to notice the suffering of others in the family.
Even though research has shown that HCW at this level can identify and report cases efficiently, they often lack the confidence to treat them. Another feature of these guidelines is that training of HCWs in providing mental health care services is not made mandatory, if a HCW chooses to provide mental health care s/he can acquire additional training in it. As mental health is one of the key components of this policy and the optionality in training will affect the quality of services provided through different centers. The underpaid health care workers may be more inclined to not undergo training as they will not receive any added incentive for it.
We need very strong coordination between the HCP of the upper and lower levels for the smooth functioning of the back referral system. This will come down to the motivation and diagnostic skills of the HCP. Incorrect diagnoses will unnecessarily burden the care seekers with agonizing travel and waiting time and discourage them from making any effort in the future. This is seen quite often in the public health care system, driving patients to lose faith in the system and to seek care at either higher levels or privately, overburdening both the higher centers and patients by increasing out of pocket expenditure.
To ensure a continuum of care the healthcare providers must be able to communicate the treatment plan, changes, and referral action at each level. This might not function effectively due to a lack of cooperation among the HCWs due to an overwhelmed workforce. Teamwork is the biggest requirement to make this policy successful. With the addition of medicine dispersion at the newer centers, a proper supply chain will have to be maintained for ensuring the availability of drugs. The challenges of sustaining a new system with adequate funding and coordination must be overcome to ensure a continuous supply of stocks. (Solanki, 2020).
Mental health differs from general health as there is no one pill to solve the problem or one size that fits all. It requires a holistic approach and regular reinforcement techniques. Therefore, what makes sense is to incorporate a positive mental health attitude from the earliest age. A critical evaluation of these guidelines would indicate that they are inadequately thought out and lack innovation. It seems repetitive and plagiarized from the same stencil used to make guidelines for other services for general health. The policy excludes the use of telecommunication services to treat mental health even though it'll be provided for other general health care services including dental healthcare. The recent coronavirus pandemic has proved the efficiency of telecommunication in treating persons with mental illnesses. The addition of this will be excellent, as specialists can communicate with the patients at the lower level without the patients having to travel and wait for long hours. To strengthen the overall public healthcare system, we need to evaluate and upgrade the higher centers as well because then the program implementation will fail due to the weaknesses within the upper tier.
The policy also leaves out an extensive list of the role and collaboration with its partner institutions such as NIMHANS and the Indian Psychiatric Institute. These institutions have been pioneering mental healthcare research and achieving successful interventions, but their role at the primary health care level is unclear within these guidelines. The policy states that the ABS for MNS guidelines are a continuation of DMHP, which is why we can assume that not all aspects of care are included in the ABS MNS guidelines, this leads to some confusion as to what all this new policy includes or excludes.
Monitoring is one of the most essential processes in estimating the burden of illness and pattern of illness. It also gives us an idea about the changing pattern of diseases and helps evaluate the outcome policy quantitatively. Poor record-keeping and lack of transparency result in deferral of the progress of the policy. The ABS policy has no provision for urgent adaptation of mental health-related HMIS indicators. Currently, only 33% of states have HMIS for mental health. (Mahajan, 2019). Lack of data will handicap the process of evaluation of the outcome of the policy and deter in recognizing the reasons for implementation failure.
Although integration of mental health at PHC is a cost-effective strategy, implementation fails due to the limitation of human and financial resources. Mental health needs to acquire a higher position in the policy agenda. Currently, India spends 1.3% of its total health budget on mental health, which is grossly inadequate keeping in mind the needs and type of reforms required. We are also short of specialists such as psychiatrists, clinical psychologists, and other social care workers. The center and states will have to increase funding for mental health care infrastructure and provision for more training institutes specifically for mental health care.
Conclusion
The burden of mental health disorders is often avoidable with early intervention, preventive, and promotive activities, and hence an efficient and constantly updating system of care at the primary level is the need of the hour. The key to eradicating the stigma around mental health is to educate the rural communities with attainable psychosocial counseling at the primary level. Community-based interventions have been successful in promoting the uptake of mental health services thereby reducing the incidences of CMDs. The policy has a lot to offer but its success will depend on constant evaluation and upgrading. Programs will have to be tailored based on the needs of the community. Attaining mental health services is frustrating not even for the poor at the rural level but also for the urban population. States will have to actively participate and increase funding towards such programs. Public-private partnerships can help address the lack of human resources and serve as a means of integrating innovation at the grass-root level. In conclusion, to ever have a realistic shot at addressing this issue we need to prioritize and constantly update policies recognizing and tackling mental health illnesses as fervently as any physical illness and universal acceptance of the problem.
Reference
Murthy, R. (2017). National mental health survey of India 2015–2016. Indian Journal of Psychiatry, 59(1), 21. https://doi.org/10.4103/psychiatry.indianjpsychiatry_102_17
Van Ginneken, N., Jain, S., Patel, V., & Berridge, V. (2014). The development of mental health services within primary care in India: learning from oral history. International Journal of Mental Health Systems, 8(1). https://doi.org/10.1186/1752-4458-8-30
Sushovan, R. & Nazish, R. (2015). The National Mental Health Programme of India. International Journal of Current Medical And Applied Sciences. 7(1), 07-15.
National Mental Health Survey (2015-16) http://www.indianmhs.nimhans.ac.in/Docs/Summary.pdf
Operational Guidelines Mental, Neurological and Substance Use (MNS) Disorders Care at Health and Wellness Centres https://ab-hwc.nhp.gov.in/download/document/Final_MNS_Operational_Guidelines_-_Web_Optimized_PDF_Version_-_19_11_20.pdf
Solanki, H. K., Rath, R. S., Silan, V., & Singh, S. V. (2020). Health and wellness centers: a paradigm shift in health care system of India? International Journal Of Community Medicine And Public Health, 7(2), 799. https://doi.org/10.18203/2394-6040.ijcmph20200470
Mahajan, P., Rajendran, P., Sunderamurthy, B., Keshavan, S., & Bazroy, J. (2019). Analyzing Indian mental health systems: Reflecting, learning, and working towards a better future. Journal of Current Research in Scientific Medicine, 5(1), 4. https://doi.org/10.4103/jcrsm.jcrsm_21_19-
(The author of the article is Ms Tooba Sayeed - an intern who worked with GRAAM from June - August, 2021).
What's Your Reaction?